Printable DNR Form New York: A Guide to End-of-Life Planning
Navigating end-of-life decisions can be complex and emotionally challenging. One crucial aspect of this process is understanding and utilizing a Do Not Resuscitate (DNR) form. In New York, DNR forms play a vital role in ensuring your wishes are respected during medical emergencies. This comprehensive guide will provide you with all the essential information about Printable DNR Form New York, empowering you to make informed decisions and plan for a dignified end-of-life experience.
We will explore the legal and ethical considerations surrounding DNR forms, guide you through the process of obtaining and completing one, and discuss the distribution, storage, and healthcare professional responsibilities related to DNR forms. Additionally, we will delve into the connection between DNR forms and advance directives, helping you create a holistic end-of-life plan that aligns with your values and preferences.
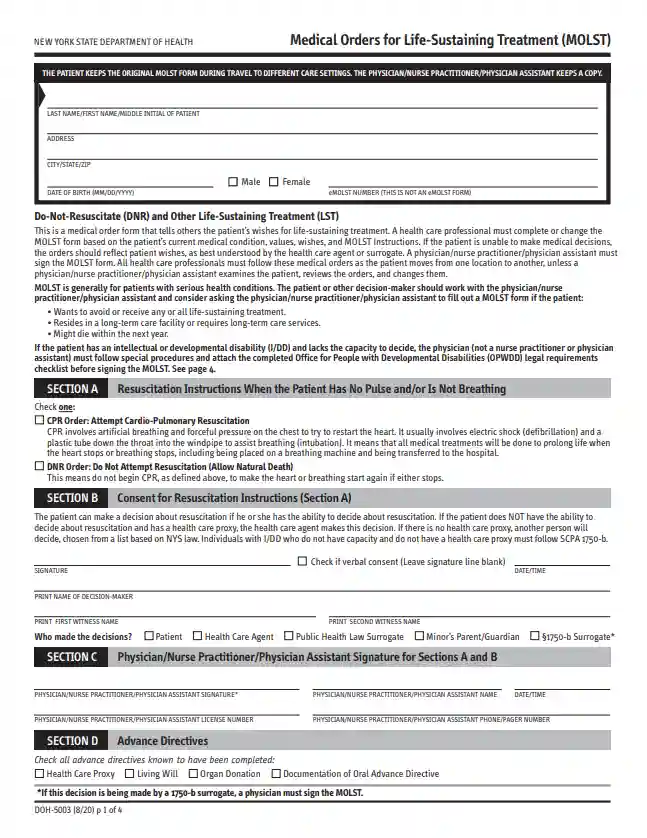
Definition and Overview
A Do Not Resuscitate (DNR) form is a legal document that expresses a person’s wishes not to receive cardiopulmonary resuscitation (CPR) or other life-sustaining treatments in the event of cardiac or respiratory arrest. DNR forms are recognized and respected by healthcare professionals in New York state and throughout the United States.
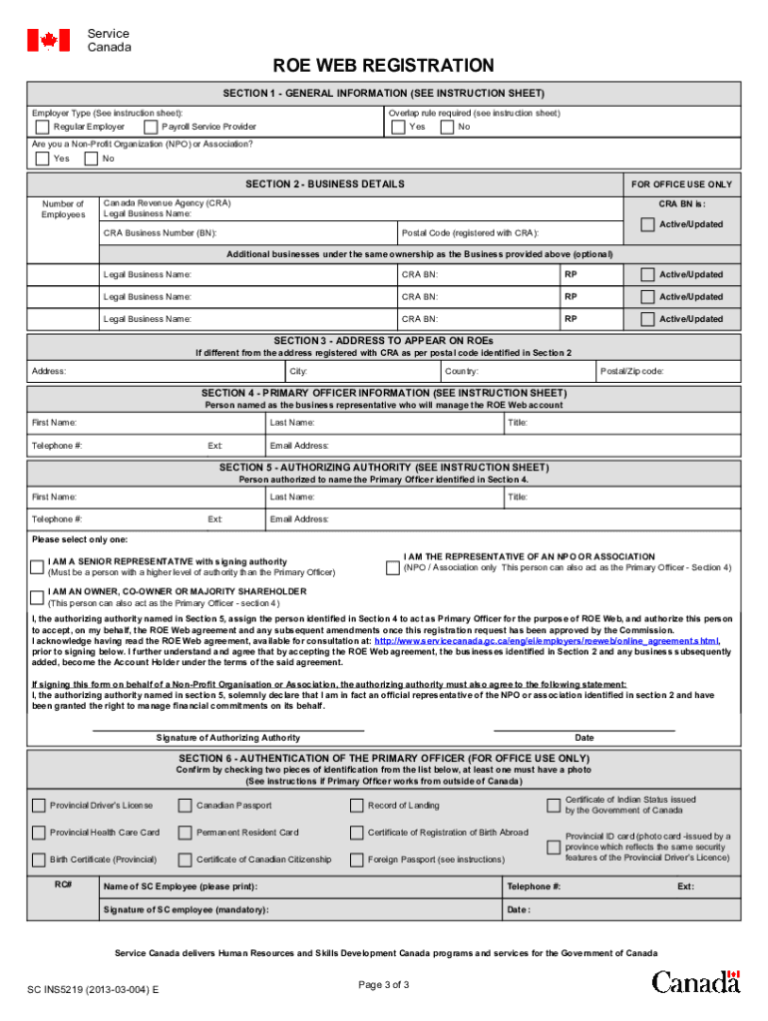
In New York, a DNR form must be signed by the individual or their healthcare proxy, and witnessed by two adults who are not related to the individual or their healthcare proxy. The form must be kept in the individual’s medical record and is valid for up to five years.
When a DNR Form May Be Used
A DNR form may be used in a variety of situations, including:
- When an individual has a terminal illness and does not wish to prolong their life.
- When an individual has a chronic condition that makes CPR or other life-sustaining treatments unlikely to be successful.
- When an individual has a strong religious or personal belief against the use of CPR or other life-sustaining treatments.
Legal and Ethical Considerations
In New York, DNR forms carry significant legal weight. The Public Health Law Article 29-C (formerly Article 40) governs the use of DNR forms and provides legal protection to healthcare providers who follow its provisions.
The ethical considerations surrounding DNR forms are complex and involve balancing the patient’s right to self-determination with the healthcare provider’s responsibility to provide life-sustaining treatment.
Role of Healthcare Professionals
Healthcare professionals play a crucial role in providing guidance on DNR forms. They are responsible for:
- Educating patients and families about DNR forms and their implications
- Assessing the patient’s capacity to make decisions about their healthcare
- Facilitating discussions between patients, families, and healthcare providers about end-of-life decisions
- Documenting the patient’s wishes in the DNR form
- Honoring the patient’s wishes when end-of-life decisions need to be made
Obtaining and Completing a DNR Form
To obtain a DNR form in New York, you can request one from your healthcare provider, hospital, or a local hospice organization. The form is typically a one-page document that includes information about your wishes regarding end-of-life care, such as whether you want to receive CPR or other life-sustaining treatments.
The DNR form will typically include the following information:
- Your name and date of birth
- Your address and phone number
- Your healthcare provider’s name and contact information
- A statement of your wishes regarding end-of-life care
- Signatures from you and two witnesses
To complete a DNR form, you will need to provide the following information:
- Your name and date of birth
- Your address and phone number
- Your healthcare provider’s name and contact information
- A statement of your wishes regarding end-of-life care
You will also need to sign the form and have it witnessed by two adults who are not related to you.
Distribution and Storage of DNR Forms
Ensuring the accessibility and proper storage of DNR forms is crucial for their effectiveness in medical emergencies.
Healthcare providers, including doctors, nurses, and paramedics, must have access to DNR forms to make informed decisions about patient care. The distribution of DNR forms should include these professionals, ensuring they are aware of the patient’s wishes and can respect their autonomy.
Entities Responsible for Maintaining DNR Forms
- Healthcare facilities, such as hospitals and nursing homes, are responsible for maintaining DNR forms and ensuring their validity.
- The patient’s primary care physician or healthcare proxy is typically responsible for completing and signing the DNR form.
- The patient’s family or legal guardian may also be involved in the process, especially if the patient is unable to make their own decisions.
Procedures for Secure Storage
- DNR forms should be stored in a secure location, such as a patient’s medical chart or a designated file cabinet.
- Access to the forms should be restricted to authorized personnel only.
- DNR forms should be regularly reviewed and updated as needed, especially if the patient’s medical condition changes.
Healthcare Professionals and DNR Forms
Healthcare professionals play a crucial role in honoring DNR forms and upholding the ethical and legal principles that govern end-of-life care. Their responsibilities encompass both respecting the patient’s wishes and ensuring their well-being.
Healthcare professionals are ethically bound to follow the instructions Artikeld in a valid DNR form, unless they believe that overriding the form is necessary to prevent harm to the patient or others. In such cases, they must carefully consider the patient’s best interests and consult with the patient’s family or legal representative.
Ethical and Legal Considerations
Healthcare professionals must navigate the ethical and legal complexities of end-of-life care with sensitivity and professionalism. They are obligated to provide compassionate care while respecting the patient’s autonomy and the law.
- Autonomy: Healthcare professionals must respect the patient’s right to make decisions about their own medical care, including end-of-life treatment.
- Beneficence: Healthcare professionals must act in the patient’s best interests, even if it conflicts with the patient’s wishes.
- Non-maleficence: Healthcare professionals must avoid causing harm to the patient.
Overriding a DNR Form
In certain exceptional circumstances, healthcare professionals may need to override a DNR form. These situations include:
- Medical error: If the DNR form was completed in error or is not valid, healthcare professionals may need to provide life-sustaining treatment.
- Emergency situations: If the patient is in immediate danger and there is no time to obtain consent, healthcare professionals may provide life-sustaining treatment.
- Patient’s best interests: If healthcare professionals believe that overriding the DNR form is in the patient’s best interests, they may do so after consulting with the patient’s family or legal representative.
Advance Directives and DNR Forms
Advance directives are legal documents that allow you to state your wishes about end-of-life care. They can include a living will, which Artikels your preferences for medical treatment, and a durable power of attorney for healthcare, which appoints someone to make medical decisions for you if you are unable to do so yourself. DNR forms are a type of advance directive that specifically states that you do not want to be resuscitated if your heart or breathing stops.
DNR forms are an important part of end-of-life planning. They can help to ensure that your wishes are respected, even if you are unable to communicate them yourself. They can also help to reduce the burden on your family and friends by making it clear what your preferences are.
Creating a Comprehensive End-of-Life Plan
If you are considering creating an advance directive, it is important to talk to your doctor or a lawyer. They can help you to understand your options and make sure that your documents are legally valid. Once you have created an advance directive, it is important to keep it in a safe place and let your family and friends know where it is. You should also review your advance directive regularly and make changes as needed.
Frequently Asked Questions
What is a DNR form?
A DNR form is a legal document that expresses your wishes not to receive cardiopulmonary resuscitation (CPR) or other life-sustaining treatments in the event of cardiac or respiratory arrest.
Why is it important to have a DNR form?
Having a DNR form ensures that your end-of-life wishes are respected, even if you are unable to communicate them yourself. It provides clear guidance to healthcare professionals and reduces the burden of decision-making for your loved ones.
How do I obtain a DNR form in New York?
DNR forms are available from various sources, including your doctor, hospital, or hospice agency. You can also download a printable DNR form from the New York State Department of Health website.
What information is included on a DNR form?
A DNR form typically includes your name, date of birth, medical diagnosis, and specific instructions regarding the medical treatments you do not wish to receive.
Who should I have witness my DNR form?
Two witnesses who are not related to you or your healthcare providers must witness your DNR form. These witnesses can be friends, family members, or members of the clergy.